From the editor: This blog is part of the weekly series we’re running during National Athletic Training Month to highlight different aspects athletic trainers should consider as they strive to provide “compassionate care for all.”
ATs work closely with patients from all walks of life, so it is imperative to have a thorough understanding of how patient values such as gender, ethnicity, socioeconomic status, religion, etc. can affect the delivery of appropriate health care. The NATA Cultural Competence Work Group, a collaborative effort between members of the NATA Ethnic Diversity Advisory Committee, LGBTQ+ Committee and the NATA Executive Committee for Education along with members from the Professional Education Committee and Professional Development Committee, was established to look more closely at this topic and provide additional resources as culturally competent care continues to evolve. The workgroup collaborated together on this content series for the March 2018 NATA News and NATA Now examining religion, implicit bias, socioeconomic status and compassionate language.
By Jennifer Volberding, PhD, ATC
As part of #NATM2018, we have discussed a variety of different views of how cultural competence influences an athletic trainer’s clinical practice. Our goal was to assist clinicians with providing high quality health care within the context the individual characteristics of both the patient and provider.1 We’ve already talked about implicit bias and the impact of religion on health care. In this blog, we’ll discuss the significant impact a patient’s financial status has on his/her overall health.
Think back to a situation in your own life where financial challenges may have impacted the choices you made in your overall life. Were you able to purchase everything you wanted at the grocery store, or were you stuck eating peanut butter and jelly sandwiches? Did you go to the doctor or the dentist regularly? Did you only purchase medication when absolutely necessary? Many of us have had to pinch pennies at different periods in our life to make a budget work, and we must remember that is the financial reality for many people and it has lasting effects on an individual’s life and health.
Now think about the many patients you have worked with. Have you ever had to ask a patient why he/she didn’t fill a prescription and the response was, “I can’t afford it”? Have you had a situation where you may be one of the only health care providers the patient has seen? Have you had parents of patients asking questions about their own health concerns and symptoms? As athletic trainers, we have a unique opportunity to make an overall impact on a patient’s life, but we need to understand the impact of socioeconomic status on the patient’s individual values, characteristics and health status.
First, it’s essential to understand how poverty (the income deemed adequate to survive), is determined by the U.S. Census Bureau and the Department of Health and Human Services.2 The poverty line or poverty threshold is important because it is the metric most agencies utilize to determine how much assistance an individual or family may receive. For example, the supplemental nutrition assistance program (SNAP) provides assistance for those under 130% of the poverty line and individuals below 138% qualify for Medicaid.2 In 2018, the income delineating the poverty line for an individual who resides in the continental United States is $12,140.2 For many, this figure is surprising low, which is why many individuals and families with obvious need do not qualify for assistance. Below you will find how the poverty line changes as the number of residents increase in a household.2
|
|
|
Income Delineating the Poverty Line*2 |
||
|
|
Individual |
Family of 2 |
Family of 3 |
Family of 4** |
|
2015 |
$11,770 |
$15,930 |
$20,090 |
$24,250 |
|
2017 |
$12,060 |
$16,240 |
$20,420 |
$24,600 |
|
2018 |
$12,140 |
$16,460 |
$20,780 |
$25,100 |
|
|
|
*Continental US Rates ** $4,320 per individual thereafter |
|
|
It is important to note, it is not just those at or below 100% of the poverty line who are at risk; many studies have demonstrated significant health impacts on those who are at or below 200% of the poverty line.3-5
Think back to your most recent preparticipation exam session. Did you have patients who didn’t have health insurance? Did that surprise you? For many with financial needs, access to health care is the first road block.
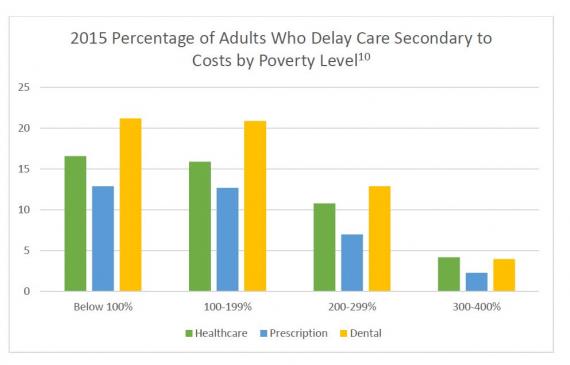
Although the Health Care Coverage and Affordable Care Act has increased the number of Americans with health insurance, many still are not covered. In 2015, 9.1% of the U.S. population (20.9 million people) were uninsured, and that number increased to 14.8% in individuals whose income was less than $75,000.6 Of those who are insured, 19.6% are covered by Medicaid and the Children’s Health Insurance Plan (CHIP), which allows for 94.7% of children to have health insurance coverage.6 Even for those who have insurance, financial constraints may impact their ability to see a physician, have a usual source of care or have adequate health care.4,7-10
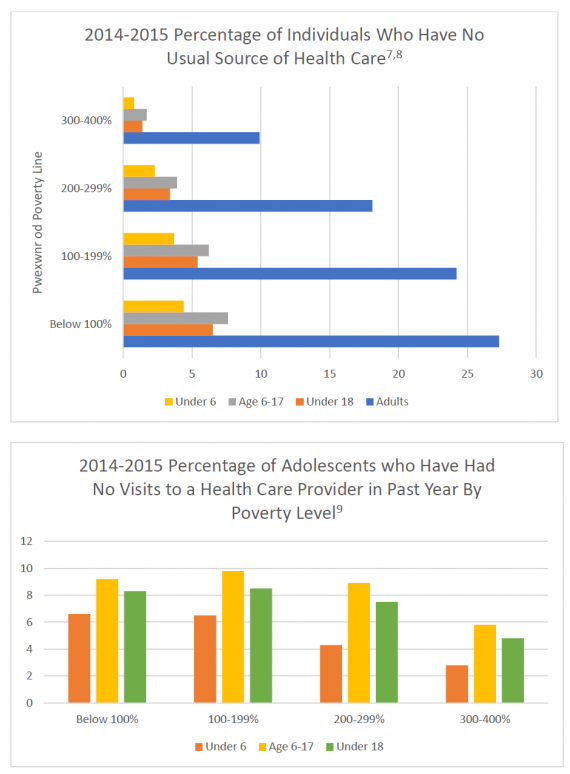
Patients at or near the poverty line are at risk for many different pathologies.1 Patients from low socioeconomic backgrounds have a life expectancy that is six years shorter than those of high financial backgrounds.3,4 Children are especially susceptible to health care disparities which can cause lifelong conditions such as psychological delays, asthma, ADHD, psychological disorders and allergies.4,5,11,12
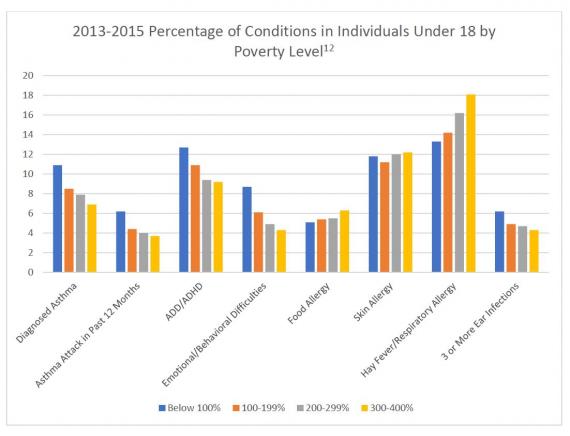
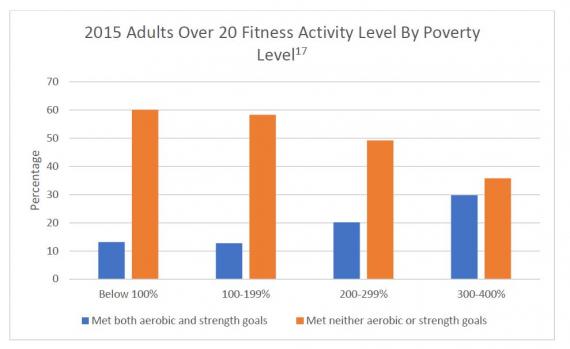
Beyond the increased susceptibility to lifelong illnesses, individuals from low socioeconomic backgrounds, especially children, are more likely to suffer from obesity and the diseases associated with being overweight or obese.4,11,13-15 This may be due to a lack of knowledge, a lack of access to healthy foods, and the high costs of fresh fruits and vegetables.15,16 The foods that are available and affordable are often processed foods that are high in fat and sugar.15 Additionally, individuals in the lower income brackets are less likely to participate in physical activities that meet the federal physical activity guidelines for Americans.17
The impact of socioeconomic status on a patient’s health status is significant. As athletic trainers, it is essential we understand our low-income patients generally have less access to health care. Understanding why a patient may not be quick to see a provider they have been referred to or fill a prescription will improve the relationship between provider and patient.
We may be the only health care provider a patient may see and the only health care provider a family has direct access to. Athletic trainers may play a role in counseling patients and their families on when it is absolutely necessary to seek out additional care, or they may provide simple assistance in dealing with non-life-threatening injuries and illnesses. It’s helpful for ATs to have knowledge of community assistance programs and services for free or low-cost care. Many hospitals and communities offer free screenings, but keep in mind that communicating this information is a very delicate conversation and should be handled with compassion.
References
-
Volberding, J. Why patient values matter in clinical decision making. NATA News. 2017:Oct:22-23.
-
Office of the Assistant Secretary for Planning and Evaluation. Poverty Guidelines web site. https://aspe.hhs.gov/poverty-guidelines. January 13, 2018. Accessed February 1, 2018.
-
Kaplan, GA, Haan, MN, Syme, SL, Mimkler, M, Winkelby, M. Socioeconomic status and health. Closing the Gap. 1987;125-129.
-
Fiscella, K, Williams, DR. Health disparities based on socioeconomic inequalities. Implications for urban health care. Academic Med. 2004:79;1139-1147.
-
Braverman, PA, Cubbin, C, Egerter, S, Williams, DR, Pamuk, E. Socioeconomic disparities in health in the United States: What the patterns tell us. Am J Pub Health. 2010:100(S1); S186-S196.
-
Barnett, JC, Vornovitsky, MS. Health insurance coverage in the United States:2015 web site. https://www.census.gov/content/dam/Census/library/publications/2016/demo/p60-257.pdf 2016. Accessed February 1, 2018.
-
Centers for Disease Control and Prevention. No usual source of health care among adults aged 18-64, by selected characteristics: United States, average annual, selected years 1993-1994 through 2014-2015 website. https://www.cdc.gov/nchs/hus/contents2016.htm#062. 2016. Accessed February 1, 2018.
-
Centers for Disease Control. No usual source of health care among children under age 18, by selected characteristics: United States, average annual, selected years 1993-1994 through 2014-2015 website. https://www.cdc.gov/nchs/hus/contents2016.htm#061 2016. Accessed February 1, 2018.
-
Centers for Disease Control and Prevention. No health care visits to an office or clinic within the past 12 months among children under age 18, by selected characteristic: United States, average annual, selected years 1997-1998 through 2014-2015 website. https://www.cdc.gov/nchs/hus/contents2016.htm#064 2016. Accessed February 1, 2018.
-
Centers for Disease Control and Prevention. Delay or nonreceipt of needed medical care, noreceipt of needed prescriptions drugs, or nonreceipt of needed dental care during the past 12 months due to cost, by selected characteristics: United States selected years 1997-2015 https://www.cdc.gov/nchs/hus/contents2016.htm#063 2016. Accessed February 1, 2018.
-
Chen, E, Shalowitz, MU, Story, RE, Erlich, KB, Levine, CS, Hayen, R, Leigh, AKK, Miller, GF. Dimensions of socioeconomic status and childhood asthma outcomes. Evidence for distinct behavioral and biological associations. Psychosomatic Med.2016:78; 1043-1052.
-
Centers for Disease Control and Prevention. Health conditions among children under age 18, by selected characteristics: United States average annual, selected years 1997-1999 through 2013-2015 web site. https://www.cdc.gov/nchs/hus/contents2016.htm#035 2016. Accessed February 1, 2018.
-
Centers for Disease Control. Normal weight, overweight, and obesity among adults aged 20 and over, by selected characteristics: United States, selected years 1988-1994 through 2011-2014 web site. https://www.cdc.gov/nchs/hus/contents2016.htm#058 2016. Accessed February 1, 2018.
-
Centers for Disease Control. Obesity among children and adolescents aged 2-19 years, by selected characteristics: United States, selected years 1988-1994 through 2011-2014 web site. https://www.cdc.gov/nchs/hus/contents2016.htm#059 2016. Accessed February 1, 2018.
-
Manyanga T, Tremblay MS, Chaput JP, Katzmarzyk PT, Fogelholm M, Hu G, Kuriyan R, Kurpad A, Lambert EV, Maher C, Maia J. Socioeconomic status and dietary patterns in children from around the world: different associations by levels of country human development? BMC Pub Health. 2017:17; 457.
-
Groeniger, JO, van Lenthe, FJ, Beenackers, MA, Kamphius, CBM. Does social distinction contribute to socioeconomic inequalities in diet the case of ‘superfoods’ consumptions. Int J Behavioral Nutrition and Physical Activity. 2017:14; 1-7.
-
Centers for Disease Control. Participation in leisure-time aerobic and muscle-strengthening activities that meet the federal 2008 Physical Activity Guidelines for Americans among adults aged 18 and over, by selected characteristics: United States selected years 1998-2015 web site. . https://www.cdc.gov/nchs/hus/contents2016.htm#057 2016. Accessed February 1, 2018.